A recent study found that electronic health records (EHRs) are creating an even greater burden on small physician practices than was originally anticipated. This study defined a small practice as one with 1-4 physicians. Published earlier this year in Perspectives in Health Information Management, this study reports that after integrating an EHR, the surveyed physicians had less time to see patients than before going paperless.
Time and Money Demands
It is estimated that approximately 90% of office-based physicians will have implemented an EHR by the end of 2017. However, due to inadequate training before and after implementation, EHRs can be a time-drain for physicians. For example, the time spent inputting data when work templates have not been optimized, cuts in to the time physicians would typically be spending with patients. The result has challenged physicians and caused dips in overall collections during times when practice expenses, like employee benefits, are skyrocketing.
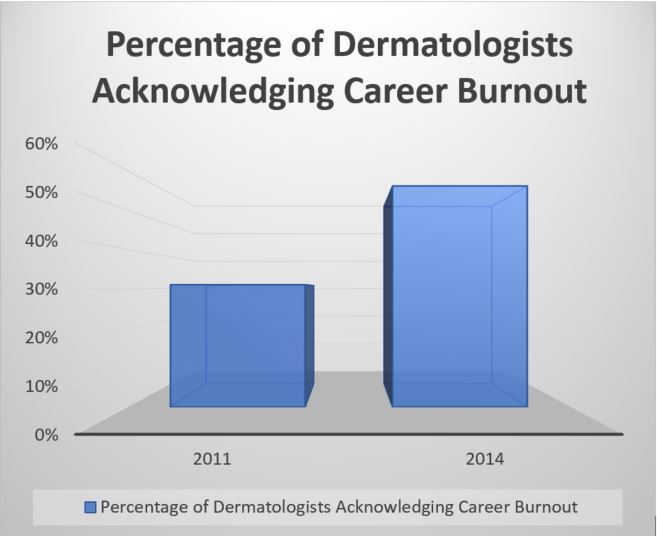
While the abovementioned study’s survey sample was limited – 15 physicians from various specialties and geographical regions – it should not be ignored. Medscape’s 2017 Lifestyle Report highlights findings from a survey of 14,000 physicians. Similarly, that survey found that increased computerization of practices is one of the top contributors to physician burnout. In fact, career burnout among dermatologists has significantly risen recently, according to a study by the Mayo Clinic.
In addition to the upfront financial and time commitment to implement an EHR system, few small practices have the internal resources necessary for ongoing IT support and security. These burdens, along with other issues like narrowing networks, are causing many dermatologists to abandon solo practice or retire early.
Need for Ongoing Support
Partnering with a quality-driven, support organization is how some smaller practices are choosing to navigate these and other industry challenges, like MACRA.
QualDerm-affiliated practices have access to a dedicated IT staff that manages the day-to-day technology issues, training and ensures each practice meets government reporting requirements.
IT support for QualDerm-affiliated practices includes:
- Customized educational materials to fit office workflows
- Classroom-based training for providers and staff
- In-house front office/clinical support desk
- Constant onsite optimization training
- MIPS Quality Assurance
As an example, to meet the new MACRA requirements, QualDerm’s IT department worked with our affiliated practices to integrate dermatology-specific categories for MIPS reporting into their EHR systems. The IT team also trained each practices’ staff to use the new system and provides on-going user support. This has allowed QualDerm-affiliated practices to collect the necessary data and puts them on track to earn a Medicare Part B reimbursement bonus. This is in sharp contrast to the 70% of other small practices that the Centers for Medicare and Medicaid Services (CMS) estimates will be penalized during the first year of MACRA reporting. What’s more, this quality data captured by QualDerm-affiliated practices can also be used when negotiating payor contracts.
Learn more about how affiliating with QualDerm can help you navigate EHRs, government reporting regulations, and other industry challenges.
Contact us to find out more about partnership opportunities or to discuss selling your practice.