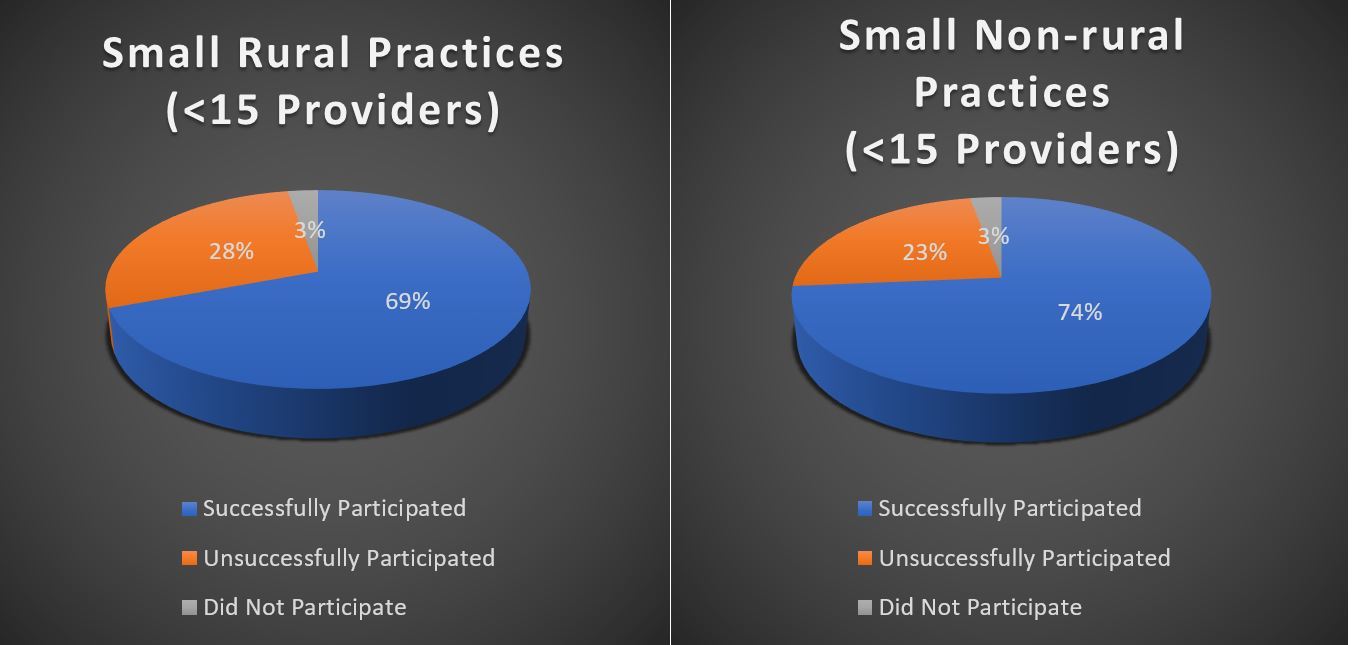
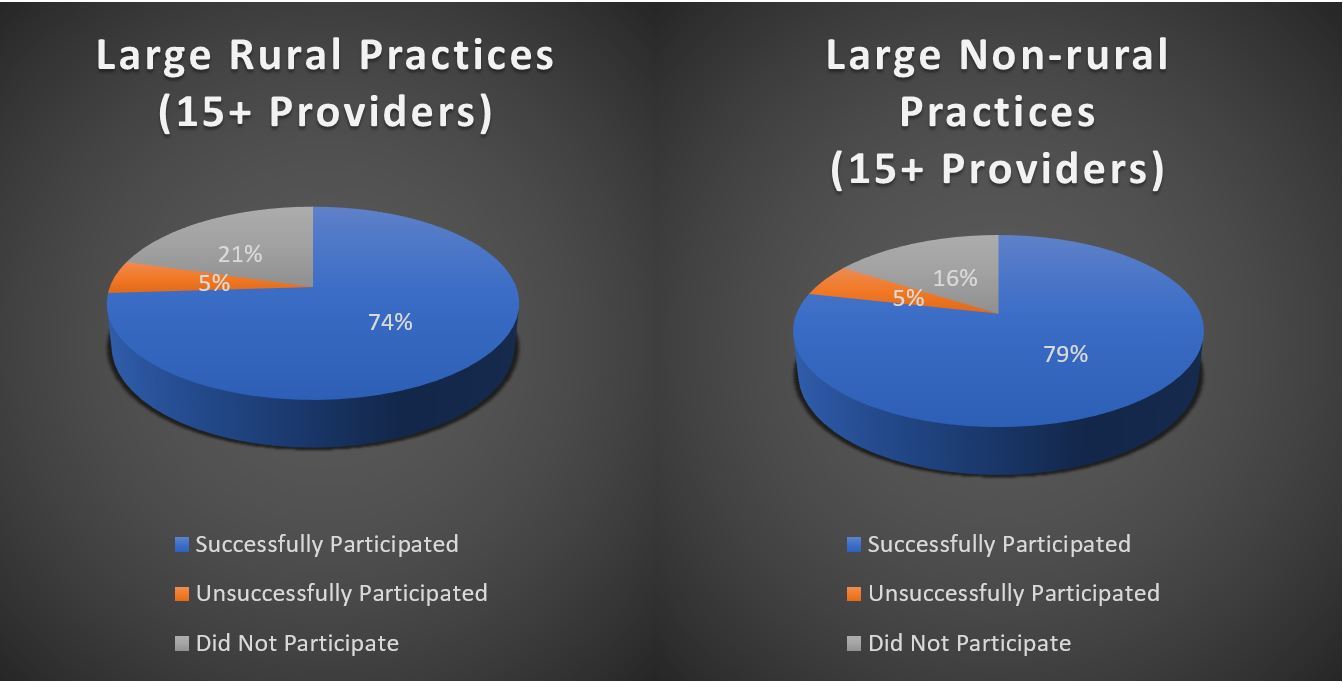
The U.S. Government Accountability Office (GAO) recently released a report highlighting the rate of which small and rural medical practices successfully participated in federally-funded payment incentive programs. The report analyzed Centers for Medicare and Medicaid Services (CMS) data from 2015, focusing on “legacy” programs – the Physician Quality Reporting System (PQRS) and Value-based Payment Modifier (VM). The report also offered a prediction of how these practices will fare under the new Merit-based Incentive Payment System (MIPS) program based on the historical data.
The variance between rural and non-rural practices was not significant, however, the GAO found larger practices did reap higher rewards than smaller ones, on average. While CMS estimates that small and rural practices will do better under MIPS, the same challenges that inhibited their success rate under legacy programs will still be a factor.
Provider Participation Rates in the Physician Quality Reporting System (PQRS)
Tech, Time, and Money
Technology and lack of staff and financial resources were identified as the top challenges small practices face in their efforts to participate in payment incentive programs. For example, purchasing and implementing electronic health records can strain both financial and staff resources. What’s more, even after implementation, staff resources are required to ensure that the reporting requirements are being met so that reimbursement penalties are avoided. Few small, independent practices have staff to spare to tackle these tasks.
QualDerm-affiliated practices have access to a dedicated IT team that manages EHR integration, upgrades, and on-going tech support. Additionally, this team customized the EHR technology to meet the specific needs of dermatology practices since the out-of-the-box data reporting functions are not specialty-specific. These efforts helped prepare QualDerm’s affiliated practices for the new MIPS requirements well in advance of the deadline, putting them on track to receive the maximum reimbursement bonus the first year.
Quality is Key
Neither the best technology, nor the most diligent data reporting will help a practice optimize incentive payments if its quality of care doesn’t meet the highest standards. Physicians understand this and have voiced concerns that unfunded government mandates are pulling them away from what should be their primary concern – caring for patients. And while many independent dermatologists are considering partnerships with larger organizations to alleviate these practice management demands, they are leery of losing their clinical autonomy, which they feel could also diminish patients’ quality of care.
Maintaining physicians’ clinical autonomy is a key element of QualDerm’s partnership model. This ensures patient care and safety remain the core focus of every QualDerm-affiliated practice. Even beyond the exam rooms, QualDerm-affiliated physicians’ input and leadership are critical in shaping the company’s policies and growth. For example, the company’s physician-led Quality Council is responsible for advancing quality of care initiatives throughout the QualDerm network.
Recently, the MIPS scores for QualDerm’s North Carolina and Ohio affiliated practices were reported. Together, QualDerm and these affiliated practices had a very successful first year under MACRA. Both The Skin Surgery Center and the Center for Surgical Dermatology and Dermatology Associates scored the highest possible MIPS score of 100% for 2017 clinical performance. These results are a testament to the benefit of high-caliber physicians working jointly with experienced business professionals to position their practices for long-term success.
Learn more about how QualDerm preserves physicians’ clinical autonomy while helping practices meet the demands of regulatory compliance.
Contact us to find out more about partnership opportunities or to discuss selling your practice.